Key Messages of the Global Health 2035 Report
On December 3, 2013, The Lancet Commission on Investing in Health (CIH) published Global Health 2035: A world converging within a generation. The report lays out a series of opportunities for donors, low-income countries, and lower-middle-income countries to achieve dramatic gains in health by 2035. Such a strategy could be funded by a combination of domestic and donor spending and a realignment of donor priorities.
The CIH report has four key messages, each accompanied by opportunities for action by national governments of low-income and middle-income countries and by the international community.
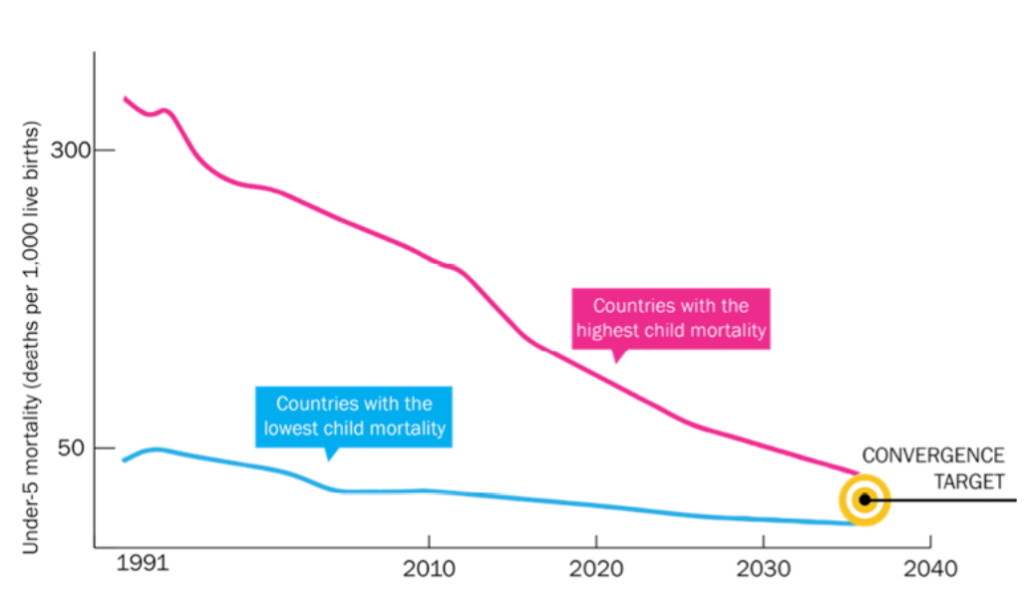
A grand convergence in health is achievable within our lifetimes
A unique characteristic of our generation is that collectively we have the financial and the ever-improving technical capacity to reduce infectious, child, and maternal mortality rates to low levels universally by 2035, to achieve a “grand convergence” in health.
With enhanced investments to scale up existing and new health interventions, and the systems to deliver them, most low-income countries and lower-middle-income countries could reduce rates of infectious, child, and maternal deaths down to levels seen today in the best-performing middle-income countries.
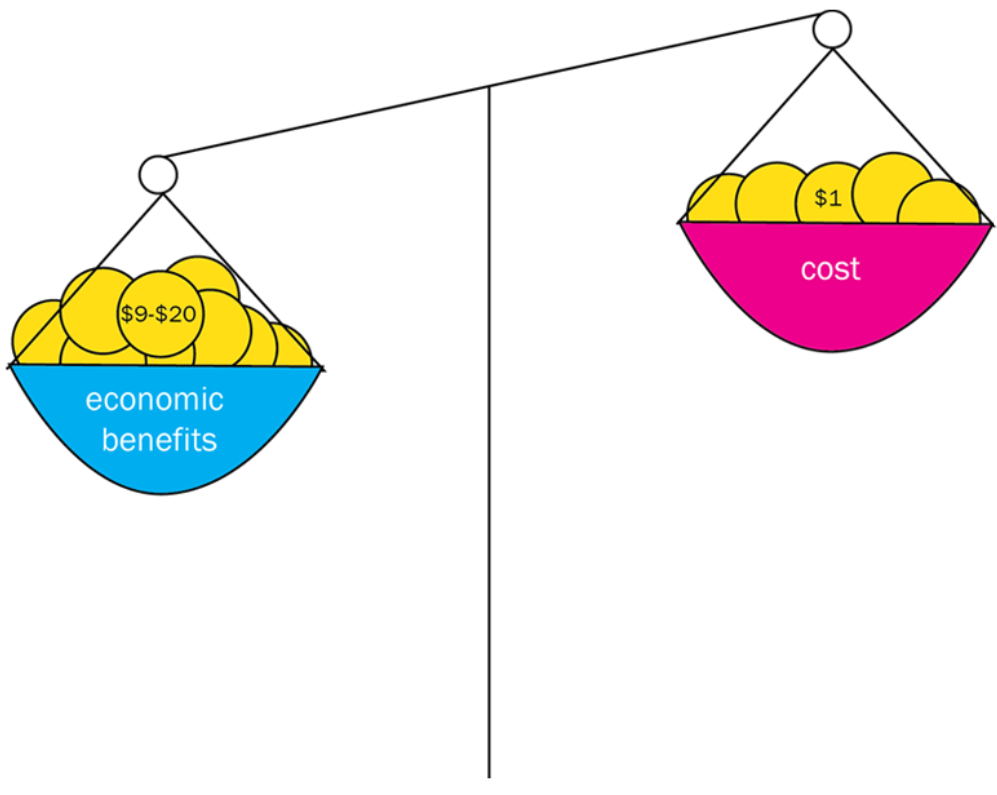
The returns on investing in health are extremely impressive
There is an enormous payoff from investing in health. Improved health contributed importantly to income growth in low-income and middle-income countries, as measured using traditional national income accounting (based on GDP). But while GDP captures the benefits that result from improved economic productivity (the so-called instrumental value of better health), it fails to capture the intrinsic value of better health—the value of health in and of itself.
Global Health 2035 reports a more comprehensive understanding of the returns to investing in health by estimating this intrinsic value using “full income” approaches. Full income approaches suggest that the intrinsic value of better health is likely to be a multiple of its instrumental value. These results provide planning ministries in low- and middle-income countries, as well as donor agencies, with a strong new rationale for increasing health spending.
Fiscal policies are a powerful, underused lever for curbing non-communicable diseases and injuries
One paradox of success in global health is that when low-income and middle-income countries successfully tackle infections and maternal and child health conditions, they then accelerate the shift in their disease burden to non-communicable disease (NCDs) and injuries in adults. The transition to NCDs and injuries is occurring because of factors such as ageing of the population and the global spread of NCD risk factors, including smoking and harmful use of alcohol.
The burden of deaths from NCDs and injuries in low-income and middle-income countries can be reduced by 2035 through inexpensive population-based and clinical interventions. Fiscal policies are an especially powerful, yet under-used, lever for reducing this burden.
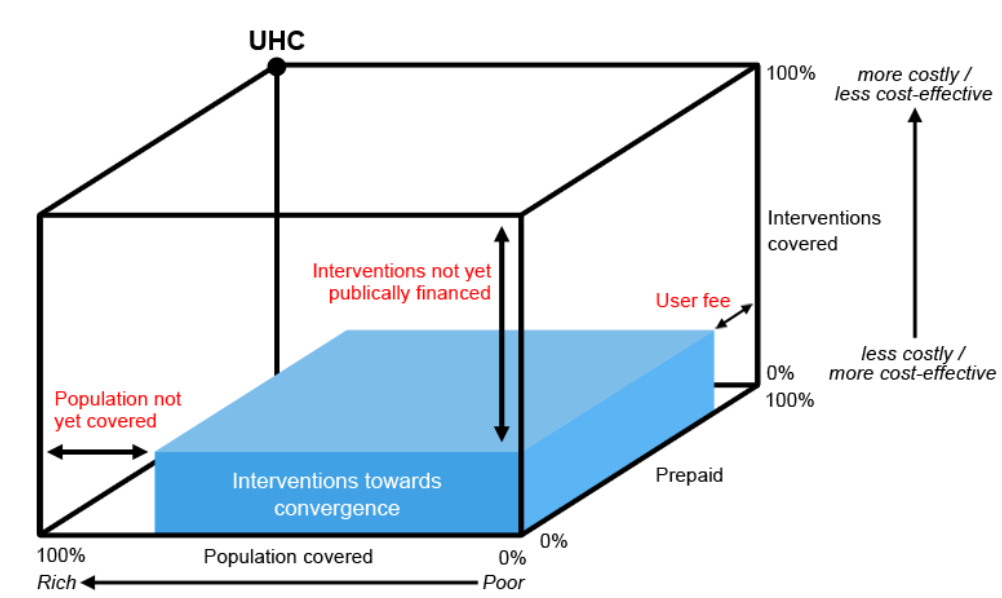
Pro-poor pathways to universal coverage are an efficient way to achieve health and financial protection
Access to essential, life-saving health interventions can be enhanced—and progress towards Global Health 2035 can be accelerated—through universal health coverage (UHC).
Global Health 2035 recommends that national governments take one of two progressive pathways toward UHC which commit to covering the poor from the outset (“progressive universalism”). In the first, publicly financed insurance would cover essential health-care interventions to achieve convergence and tackle NCDs and injuries. This pathway would directly benefit the poor, since they are disproportionately affected by these problems. The second pathway provides a larger benefit package, funded through a range of financing mechanisms (e.g. payroll taxes, insurance premiums, copayments), with poor people exempted from all payments.